GDS 2020: Medical cannabis: So much promise, but the evidence is still thin. Can you help?
Professor Adam R Winstock, Consultant Psychiatrist and CEO, GDS
As medical cannabis becomes regulated and available via a physician’s recommendation (in the USA) or a prescription in other countries, the possibilities and promise that cannabis derived medicines offer is huge. Huge not only for the human suffering this complex plant may ameliorate, but for the pharma companies, doctors and clinics that will inevitably profit from the industry’s growth.
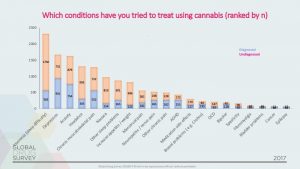
In GDS2017 we asked people why they used cannabis and for those advising their use as medical, we asked what conditions were being treated. The results are summarised below.
The findings are based on a sample of 5000 recent medical cannabis consumers.
It’s worth noting that the majority were treating a condition that had not been diagnosed by a doctor and that mental health related disorders came out top. These two points are really important. First asking psychiatrists to believe that cannabis is good for people with mental health disorders is like convincing people who run Weightwatchers that pizza is a good diet food. Second is the difference between self-diagnosis and actual diagnosis. The two are not always the same. Making an inaccurate self-diagnosis and masking the symptoms with cannabis could delay people seeking out an assessment and treatment by a healthcare professional.
Self-diagnosis of conditions such as anxiety might mean that diseases such an overactive thyroid or underlying heart problem might be missed. To top this all off, we found that almost 70% of those trying to seek to manage their own health with cannabis, had not disclosed their medical use to their doctor, typically because they thought their doctor would have nothing useful to offer or would view such use negatively. That was a bit depressing.
So, what’s the reality about cannabis as medicine? There is no simple answer because there are over 140 active cannabinoids in the plant, their actions are diverse, are modulated by the presence of each other and by the route of administration – and that’s before we start talking about potency and dose. There is research of reasonable quality that supports the use of cannabis products for some sorts of chronic pain, spasticity and nausea associated with chemotherapy. The evidence is not huge and many authoritative groups (see below) regard the evidence as pretty light, variable and inconsistent, with much of it not supported by good randomised clinical trials.
The evidence for cannabis as being effective as a treatment for common psychiatric conditions such as depression, anxiety or PTSD are to date limited. A review of trials (many of poor quality with no control groups) conducted over the last 40 years, published in Lancet Psychiatry at the end of October 2019, concluded that the risks outweighed the benefits. Only among those patients with multiple sclerosis or chronic pain and who reported using cannabis to help with co-existing anxiety was the evidence considered not to be of low quality.
To those who use cannabis to improve their health and well-being, the outcomes of studies that don’t support their lived experience is frustrating. This is especially the case for those with common psychiatric conditions such as anxiety and depression, where traditional psychiatrist medications may be unattractive. Do the trial results mean your reported benefits are not genuine? Nope
One of the other things that makes cannabis difficult to study is that in many conditions its diverse effects may benefit a number of discreet symptoms associated with a disease. For example in chronic pain, cannabis (or THC or CBD or something else in the plant) may not only help to dampen pain signals but might help with sleep and anxiety which are common in those with pain. The same issue goes for those with PTSD for example. In fact, the whole issue of there being limited research is a debate in itself with many groups suggesting approaches other than RCTs are not the only way to find the answers. For example, we could be looking at patient registries and learning from small open label studies.
But we can also compile what we know already from the experiences of 1000s of people who use cannabis products to help with their emotional and physical health. GDS2020 aims to become one of the biggest ever studies of medical cannabis. We can learn so much from the lived experience of people.
So, if you have used cannabis to help manage a medical condition, please take some time to share your experiences and take part in now GDS2020: www.globaldrugsurvey.com/GDS2020
We’ll share what we learn to help the world understand how and why cannabis for some people may be useful.